Abstract
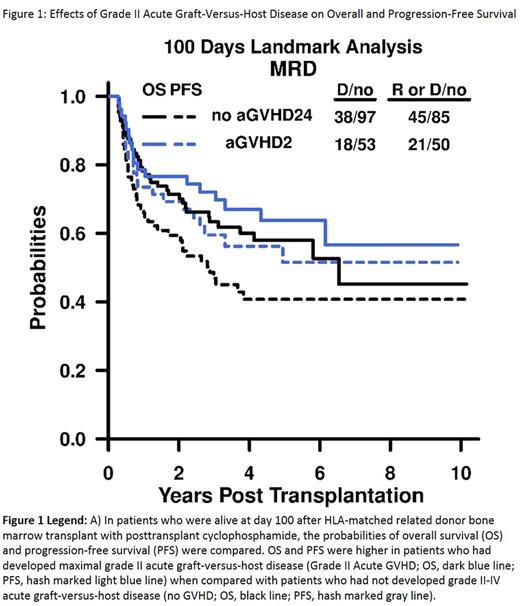
Introduction: Posttransplant cyclophosphamide (PTCy) can be safely utilized as the sole graft-versus-host-disease (GVHD) prophylaxis after myeloablative conditioning (MAC) for HLA-matched bone marrow transplant (BMT). However, the effects of GVHD with this transplant platform are not well defined. Methods: We retrospectively analyzed 298 consecutive adult patients transplanted between 2004-2012 for hematologic malignancy who engrafted after MAC (busulfan with either fludarabine or Cy) HLA-matched related (MRD, n=187) or HLA-matched unrelated (MUD, n=111) T-cell-replete BMT with Cy 50 mg/kg on days 3 and 4. Results: Median recipient age was 48 and 47 years for MAC MRD and MUD BMT, respectively. Median follow up was 4.33 and 3.74 years in the two cohorts, respectively. After MAC MRD BMT, 35% of patients experienced grade II acute (a) GVHD, 12% grade III-IV aGVHD, and 9% chronic (c) GVHD. After MAC MUD BMT, 54% of patients experienced grade II aGVHD, 17% grade III-IV aGVHD, and 17% cGVHD. We choose landmark analyses that look at the time to an event after a pre-specified time point. By starting the failure-time clock later, one can regard events prior to the landmark as baseline factors in the analysis, allowing us to study the effects of a posttransplant event on subsequent outcomes. We selected landmark time points at 100 days and 1 year, which allowed us to capture 100% of the patients who developed maximal grade II aGVHD and 97% of the patients who developed cGVHD. Few patients died of acute or chronic GVHD before their respective landmark time points. In landmark analyses at 100 days after MAC MRD BMT, 4-year overall survival (OS) and progression-free survival (PFS) were 60% (95% CI: 0.50-0.72) and 41% (95% CI: 0.30-0.54) in patients without grade II-IV aGVHD, and 67% (95% CI: 0.55-0.82) and 56% (95% CI: 0.43-0.73) in patients with maximal grade II aGVHD (Figure 1). In landmark analyses at 100 days after MAC MUD BMT, 4-year OS and PFS were 51% (95% CI: 0.36-0.73) and 44% (95% CI: 0.28-0.69) in patients without grade II-IV aGVHD, and 65% (95% CI: 0.52-0.82) and 45% (95% CI: 0.31-0.64) in patients with grade II aGVHD. In landmark analysis at 1 year after MAC MRD BMT, 4-year OS and PFS were 77% (95% CI: 0.67-0.89) and 60% (95% CI: 0.46-0.77) in patients without GVHD, and 69% (95% CI: 0.45-1) and 75% (95% CI: 0.5-1) in patients with cGVHD. In landmark analysis at 1 year after MAC MUD BMT, 4-year OS and PFS were 57% (95% CI: 0.39-0.82) and 57% (95% CI: 0.36-0.90) in patients without GVHD, and 90% (95% CI: 0.73-1) and 75% (95% CI: 0.5-1) in patients with cGVHD. In time-dependent multivariable analyses adjusted for disease risk index, recipient age, and hematopoietic cell transplant-comorbidity index (HCT-CI), grade II aGVHD was associated with improved OS and PFS after both MAC MRD (HR 0.56 95% CI 0.3-1.05, p=.07 and HR 0.59 95% CI 0.35-0.99, p=.05, respectively) and MAC MUD BMT (HR 0.53 95% CI 0.26-1.06, p=.07 and HR 0.47 95% CI 0.25-0.91, p=.03, respectively). In contrast, after MAC MRD, grade III-IV aGVHD was associated with decreased OS (HR 2.25 95% CI 1.18-4.29, p=.01) with no significant difference in PFS (HR 1.5 95% CI 0.8-2.81, p=.20). In contrast to the univariable analysis, chronic GVHD was not significantly associated with OS or PFS in MAC MRD (HR 1.18 95% CI: 0.52-2.69, p=.69 and HR 0.77 95% CI: 0.34-1.74, p=.53) or MAC MUD (HR 0.73 95% CI: 0.27-1.97, p=.53 and HR 0.67 95% CI: 0.28-1.65, p=.39) BMT. Increasing nucleated cell graft dose as a continuous variable was associated with improved PFS after MAC MRD and MAC MUD BMT (HR 0.85 95% CI 0.71-1.01, p=.06 and HR 0.83 95% CI 0.69-1.0, p=.05, respectively). Conclusion: Development of maximal grade II aGVHD was associated with significantly improved PFS after HLA-matched BMT with PTCy. In this distinct cohort, we validated prior work from our group, which showed that grade II aGVHD improves PFS after nonmyeloablative HLA-haploidentical BMT with PTCy, mycophenolate mofetil, and tacrolimus (McCurdy et al. 2017 submitted for publication). This suggests that, in the setting of PTCy, grade II aGVHD improves PFS. Therefore intensifying GVHD prophylaxis to reduce grade II aGVHD may not improve transplant outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal